With the demand for human organs greatly outweighing the supply available, the scientific and healthcare communities have needed to make strides in creating alternative solutions to aid sick patients. Xenotransplantation is one such development that aims to avoid the uncertainty and mortality risk associated with waiting for lifesaving organ transplants.

What is Xenotransplantation?
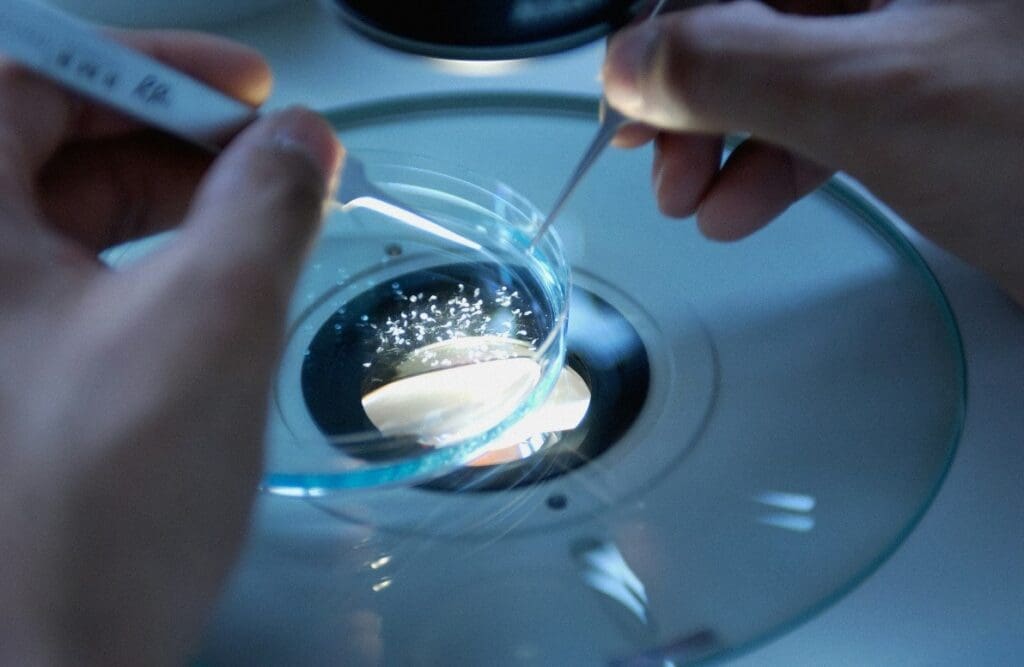
Xenotransplantation is any procedure in which live cells, tissues, or organs from a nonhuman animal source are transplanted, implanted, or infused into a human recipient. This also includes human body fluids, cells, tissues, or organs that have had outside contact with live nonhuman animal cells, tissues, or organs. It is a tentative answer to those waiting for vital organ transplants and has hopes of decreasing patient deaths. Some of the more common species used for xenotransplantation include pigs, monkeys, chimpanzees, and baboons.
The Benefits of Xenotransplantation
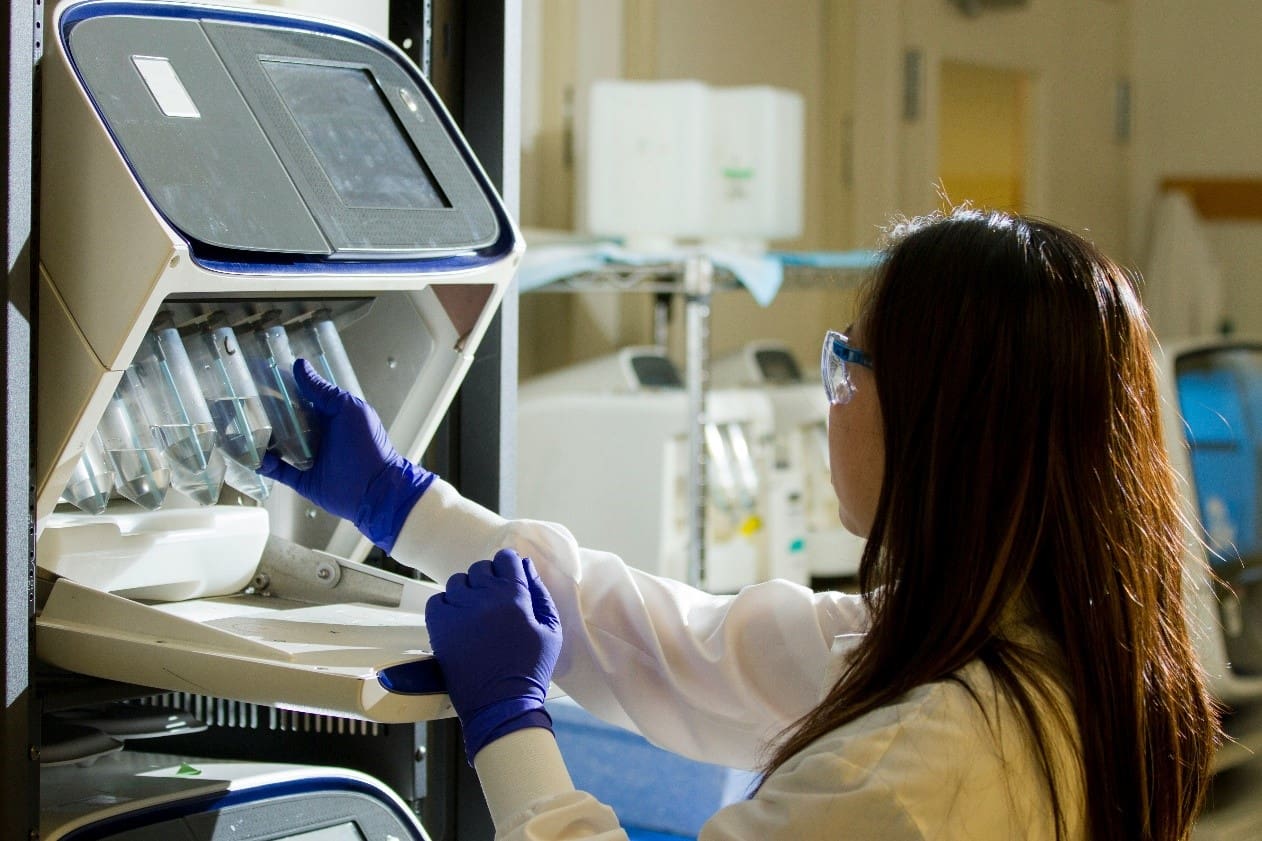
Porcine xenotransplantation has become the prime interest in recent years due to the pigs’ organ size, metabolism, and immune system most similarly resembling humans. The increased availability of pigs greatly expands the supply of organs for transplantation, making immediate transplant surgery possible for patients in urgent situations. Furthermore, with the pigs being raised and closely monitored in ideal environments, the risk of pathogen transfer is significantly reduced.
The Potential Therapeutic Effects of Xenotransplantation
Hematologic disorders: Hematologic disorders are conditions found in the blood and blood-forming organs. Xenotransplantation is beneficial for patients with leukemia, lymphoma, and sickle cell anemia who rely on red blood cells and a bone marrow transplant for survival.
Neurodegenerative diseases: Neurodegenerative diseases such as Parkinson’s and Huntington’s are optimal targets for xenotransplantation to replace lost neurons. This would be a significant breakthrough because most medications targeted toward neurodegenerative disorders only help with associated symptoms.
Cortical and neuro-retinal blindness: Xenotransplantation can be useful in replacing damaged eye tissues that cause cortical blindness.
End-stage pulmonary, cardiac, hepatic, and renal diseases: These organs significantly lose their function when irreversibly impaired. With the life expectancy being anytime between a few months to a couple of years during the end-stage, xenotransplantation can be an option for a lifesaving organ transplant.
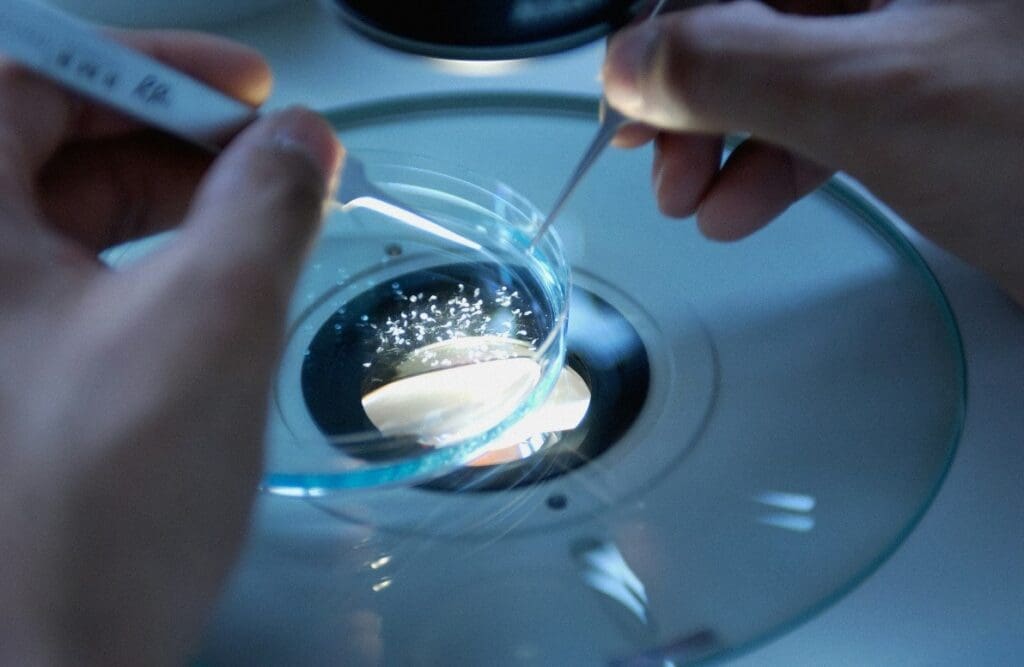
Diabetes mellitus: Damaged pancreatic islets (which are responsible for adequate hormone production to maintain appropriate circulating glucose levels) can be replaced using xenotransplantation. This is particularly lifesaving in patients with Type I diabetes mellitus who depend on insulin.
The Concerns with Xenotransplantation
While the benefits of xenotransplantation are substantial, there are concerns regarding potential infectious agents that may or may not be recognized by human recipients post-transplantation. This can also spread to the recipients’ close contacts and even to the general human population. One of the greatest concerns is the possibility of cross-species infection by retroviruses, which can remain dormant and manifest as diseases years later. If new, unknown infectious agents emerge, they may be difficult to identify with current techniques and technologies. Furthermore, transplantation is usually associated with immunosuppressant drug administration. These drugs lower a patient’s ability to fight off infections and increase the risk of contamination.
Another concern regarding xenotransplantation that proves to be its biggest barrier is the issue of rejection. Our bodies have natural responses to recognize something foreign to us. Rejection could cause numerous problems and the patient’s cells can start attacking the new unfamiliar cell, tissue, or organ. While there have been strides in lessening the likelihood of xenotransplant rejection, organ rejection can occur in any circumstance. Most solutions for this are still in the early stages of development.
Conclusion
Xenotransplantation is early in its journey to becoming a standard medical procedure for patients with organ failure. There is much to gain from its success, but valid concerns and barriers must be overcome before it is fully established. The latest research proves promising for the future and it may only be a few years before more patients can start receiving the lifesaving procedures they need.
Breaking Barriers: The Promise of Xenotransplantation
With the demand for human organs greatly outweighing the supply available, the scientific and healthcare communities have needed to make strides in creating alternative solutions to aid sick patients. Xenotransplantation is one such development that aims to avoid the uncertainty and mortality risk associated with waiting for lifesaving organ transplants.

What is Xenotransplantation?
Xenotransplantation is any procedure in which live cells, tissues, or organs from a nonhuman animal source are transplanted, implanted, or infused into a human recipient. This also includes human body fluids, cells, tissues, or organs that have had outside contact with live nonhuman animal cells, tissues, or organs. It is a tentative answer to those waiting for vital organ transplants and has hopes of decreasing patient deaths. Some of the more common species used for xenotransplantation include pigs, monkeys, chimpanzees, and baboons.
The Benefits of Xenotransplantation
Porcine xenotransplantation has become the prime interest in recent years due to the pigs’ organ size, metabolism, and immune system most similarly resembling humans. The increased availability of pigs greatly expands the supply of organs for transplantation, making immediate transplant surgery possible for patients in urgent situations. Furthermore, with the pigs being raised and closely monitored in ideal environments, the risk of pathogen transfer is significantly reduced.
The Potential Therapeutic Effects of Xenotransplantation
Hematologic disorders: Hematologic disorders are conditions found in the blood and blood-forming organs. Xenotransplantation is beneficial for patients with leukemia, lymphoma, and sickle cell anemia who rely on red blood cells and a bone marrow transplant for survival.
Neurodegenerative diseases: Neurodegenerative diseases such as Parkinson’s and Huntington’s are optimal targets for xenotransplantation to replace lost neurons. This would be a significant breakthrough because most medications targeted toward neurodegenerative disorders only help with associated symptoms.
Cortical and neuro-retinal blindness: Xenotransplantation can be useful in replacing damaged eye tissues that cause cortical blindness.
End-stage pulmonary, cardiac, hepatic, and renal diseases: These organs significantly lose their function when irreversibly impaired. With the life expectancy being anytime between a few months to a couple of years during the end-stage, xenotransplantation can be an option for a lifesaving organ transplant.
Diabetes mellitus: Damaged pancreatic islets (which are responsible for adequate hormone production to maintain appropriate circulating glucose levels) can be replaced using xenotransplantation. This is particularly lifesaving in patients with Type I diabetes mellitus who depend on insulin.
The Concerns with Xenotransplantation
While the benefits of xenotransplantation are substantial, there are concerns regarding potential infectious agents that may or may not be recognized by human recipients post-transplantation. This can also spread to the recipients’ close contacts and even to the general human population. One of the greatest concerns is the possibility of cross-species infection by retroviruses, which can remain dormant and manifest as diseases years later. If new, unknown infectious agents emerge, they may be difficult to identify with current techniques and technologies. Furthermore, transplantation is usually associated with immunosuppressant drug administration. These drugs lower a patient’s ability to fight off infections and increase the risk of contamination.
Another concern regarding xenotransplantation that proves to be its biggest barrier is the issue of rejection. Our bodies have natural responses to recognize something foreign to us. Rejection could cause numerous problems and the patient’s cells can start attacking the new unfamiliar cell, tissue, or organ. While there have been strides in lessening the likelihood of xenotransplant rejection, organ rejection can occur in any circumstance. Most solutions for this are still in the early stages of development.
Conclusion
Xenotransplantation is early in its journey to becoming a standard medical procedure for patients with organ failure. There is much to gain from its success, but valid concerns and barriers must be overcome before it is fully established. The latest research proves promising for the future and it may only be a few years before more patients can start receiving the lifesaving procedures they need.