Genetic Testing for Prostate Cancer
Prostate cancer is one of the most common cancers among men worldwide and represents a significant public health concern. Advances in genetics have transformed the understanding of this disease, shifting prostate cancer care from a uniform approach to one increasingly guided by molecular insight. Genetic testing, which identifies inherited or acquired mutations that increase risk or affect treatment response, has emerged as a central tool in precision medicine. This article examines the role of genetic testing in prostate cancer, its clinical implications, and the challenges that accompany its integration into modern healthcare.

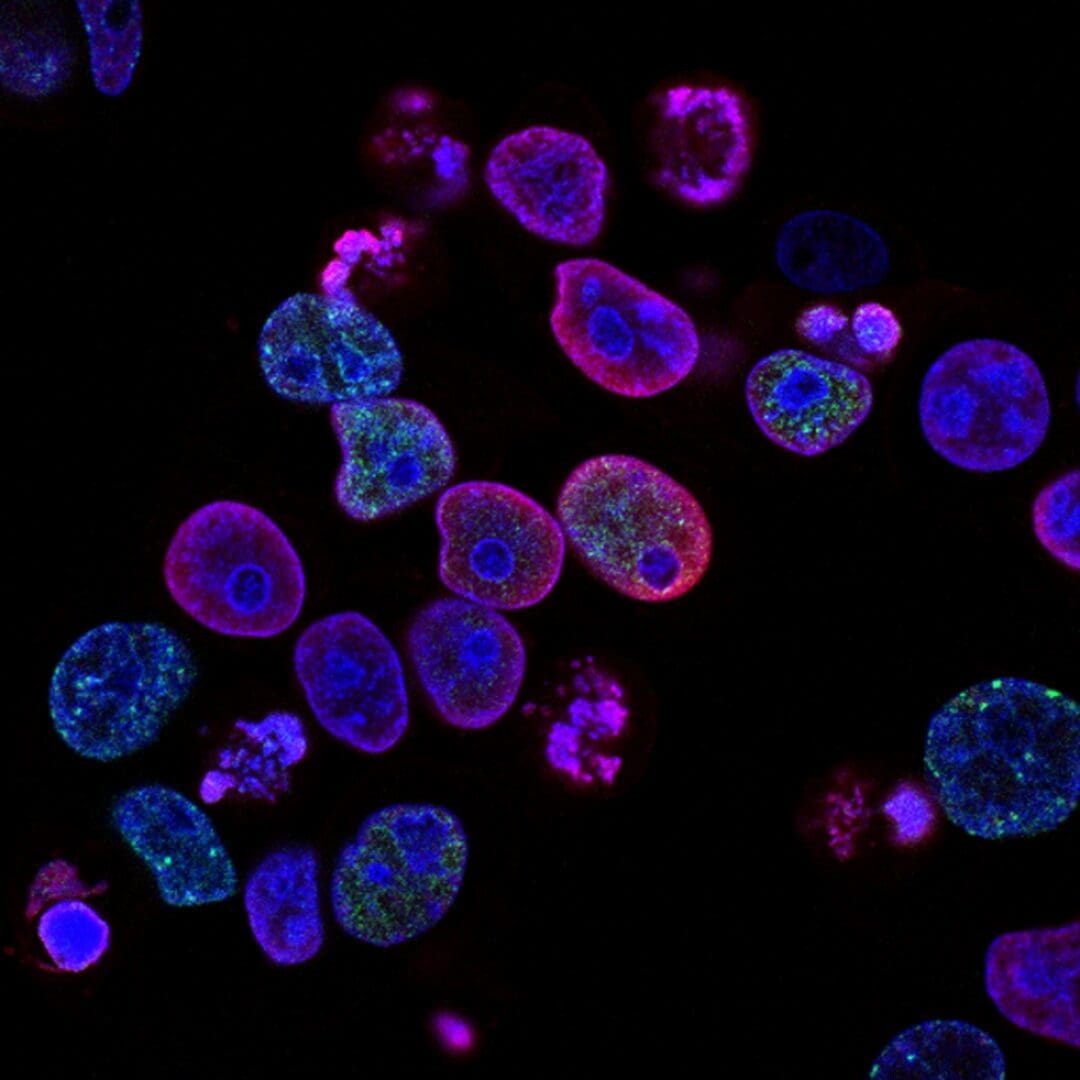
Prostate cancer develops through a combination of environmental and hereditary factors. While age, race, and diet influence risk, approximately 5 to 10 percent of all prostate cancer cases are associated with inherited mutations. The most well-established genes linked to prostate cancer include BRCA1, BRCA2, HOXB13, ATM, CHEK2, and mismatch repair genes such as MLH1, MSH2, MSH6, and PMS2. Men with BRCA2 mutations face a two- to six-fold higher risk of developing prostate cancer, often at a younger age and with more aggressive features. Identifying these genetic variants enables clinicians to identify individuals who may benefit from earlier and more frequent screening, thereby improving outcomes through timely detection. Somatic mutations that arise in tumor cells can also inform treatment decisions, as genetic sequencing of tumor tissue can identify mutations that predict response to targeted therapies such as PARP inhibitors or immunotherapy.
Genetic testing offers valuable applications throughout the continuum of prostate cancer care. For men with a strong family history, germline testing offers insight into inherited risks and enables relatives to consider cascade testing. For those already diagnosed, molecular profiling refines prognosis and guides therapy. For example, tumors with DNA repair defects may respond favorably to PARP inhibitors, such as olaparib. In contrast, patients with mismatch repair deficiencies may be eligible for immune checkpoint inhibitors. Beyond individual care, genetic testing contributes to precision oncology by linking genomic data to clinical outcomes. These insights enable researchers and clinicians to develop new therapeutic targets and optimize treatment algorithms.
Despite its promise, the implementation of genetic testing in prostate cancer faces several obstacles. Cost and inconsistent insurance coverage remain significant barriers, particularly for patients with limited access to healthcare. The interpretation of genetic results also requires specialized expertise, yet there is a national shortage of trained genetic counselors. Ethical concerns, including anxiety over hereditary risk and fear of genetic discrimination, continue to influence patients’ willingness to undergo testing. Although the Genetic Information Nondiscrimination Act offers legal protection, misconceptions persist. Moreover, racial and socioeconomic disparities contribute to unequal access to testing, particularly among populations that already experience higher prostate cancer mortality. Ensuring affordable and equitable access to both testing and counseling is essential to maximizing the benefits of genetic medicine.

As precision medicine evolves, the integration of genetic testing into prostate cancer care will continue to expand. Routine genetic screening for high-risk individuals and tumor sequencing for advanced cases are likely to become standard practice. Future research should focus on improving test affordability, strengthening genetic counseling infrastructure, and increasing public awareness. Genetic testing represents a significant advancement in prostate cancer prevention and treatment by enabling earlier detection, personalized therapy, and informed family planning. However, its full potential can only be achieved through policies that promote equity, education, and access. Through continued investment and awareness, genetic testing can help shift medicine toward a more preventive and patient-centered model of care.